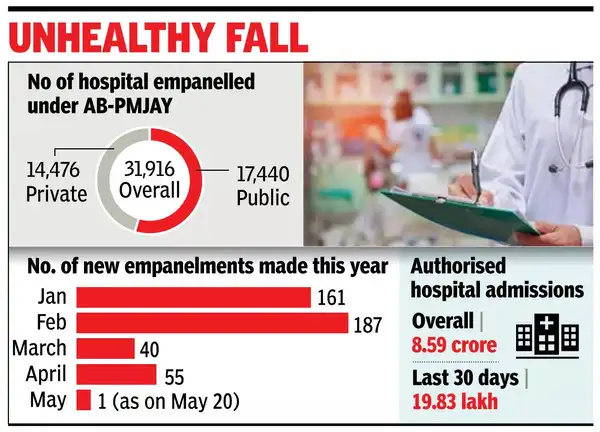
NEW DELHI: Empanelment of hospitals under the Ayushman Bharat-PM Jan Arogya Yojana has dropped significantly, from an average of 316 per month in 2024 to 111 per month in 2025, as of April.Data shared by National Health Authority (NHA) on scheme’s dashboard shows that 443 hospitals were empanelled under the AB-PMJAY across India in four months – 161 in Jan, 187 in Feb, 40 in March and 55 in April. In May, the latest update shows, 20 hospitals were empanelled.Many healthcare associations point out that low package rates and delayed payments are key reasons behind the lukewarm response to government schemes from the private sector, especially large corporate hospital chains.However, a senior official of NHA – the implementing agency of the AB-PMJAY – said empanelment is taking place and that some of the new empanelments may not have been updated as they were migrating to a new system.
AB-PMJAY, which is available in all states/UTs, except West Bengal, offers treatment worth Rs 5 lakh and, in some cases, more, per family for treatment of nearly 2,000 procedures involving specialties, including medical oncology (cancer treatment), emergency care, orthopaedic and urology (kidney-related ailments).The CEO of a top hospital chain in Delhi, the latest state to join the scheme, told TOI that package rates offered for various procedures under the AB-PMJAY were lower than their input cost. “We may join the scheme if the package rates are increased,” he said.The Indian Medical Association has also stressed on the need to increase package rates to make treatment under the scheme more sustainable. “The rates should be raised to at least CGHS level,” said an IMA office-bearer.As many as 609 private hospitals have opted out of the scheme since 2018, minister of state for health Prataprao Jadhav said in a written response to a Parliament question in March. “The reasons for hospitals voluntarily opting out include empanelment only for Covid period, hospitals were closed or non-functional, changes in hospital entity, hospital relocated, ongoing reconstruction or renovation, unavailability of specialist doctors, voluntary withdrawal from scheme, package rates, opting out due to certain treatment packages reserved for public hospitals only (Chhattisgarh and Gujarat), and no referral from public hospitals (Karnataka),” he added.



